Food Allergy Conundrums: Right Meal to Right Person
by Ingrid Roche, Senior Project Officer, National Allergy Council
So a patient or resident has food allergy. You have chosen safe foods for them, checked all ingredients and prepared the meal safely to prevent cross contamination with food allergens. Now you need to make sure that the right meal gets to the right person - the final important step!
Most allergic reactions in foodservice happen when someone is given a food or ingredient they are allergic to, and one way this can happen is by being given the wrong meal.
Hospital meals may be delivered by foodservice attendants, patient care attendants and other support staff, or nurses. In aged care facilities it could be foodservice staff, care staff or nursing staff. Meals might be individually plated and delivered to the patient’s or resident’s room. They may also be delivered in the dining room with individually plated meals or buffet style. Whatever the delivery method, foodservice staff must always have processes in place that make sure the right meal is given to the right person.
With our foodservice working group, here is what we’ve identified as best practice for meal delivery in health care settings:
1. Train all staff in food allergy, relevant to their role. Everyone involved in foodservice and delivering meals to the patients or residents must be trained to understand food allergies and food allergen management, and know the meal delivery procedures in the facility they work in.
- Only staff who have completed food allergy training should deliver meals to patients or residents with food allergy.
2. Meals for patients or residents with food allergy should stand out from other meals so that it is easy for staff to see that it is a food allergy meal.
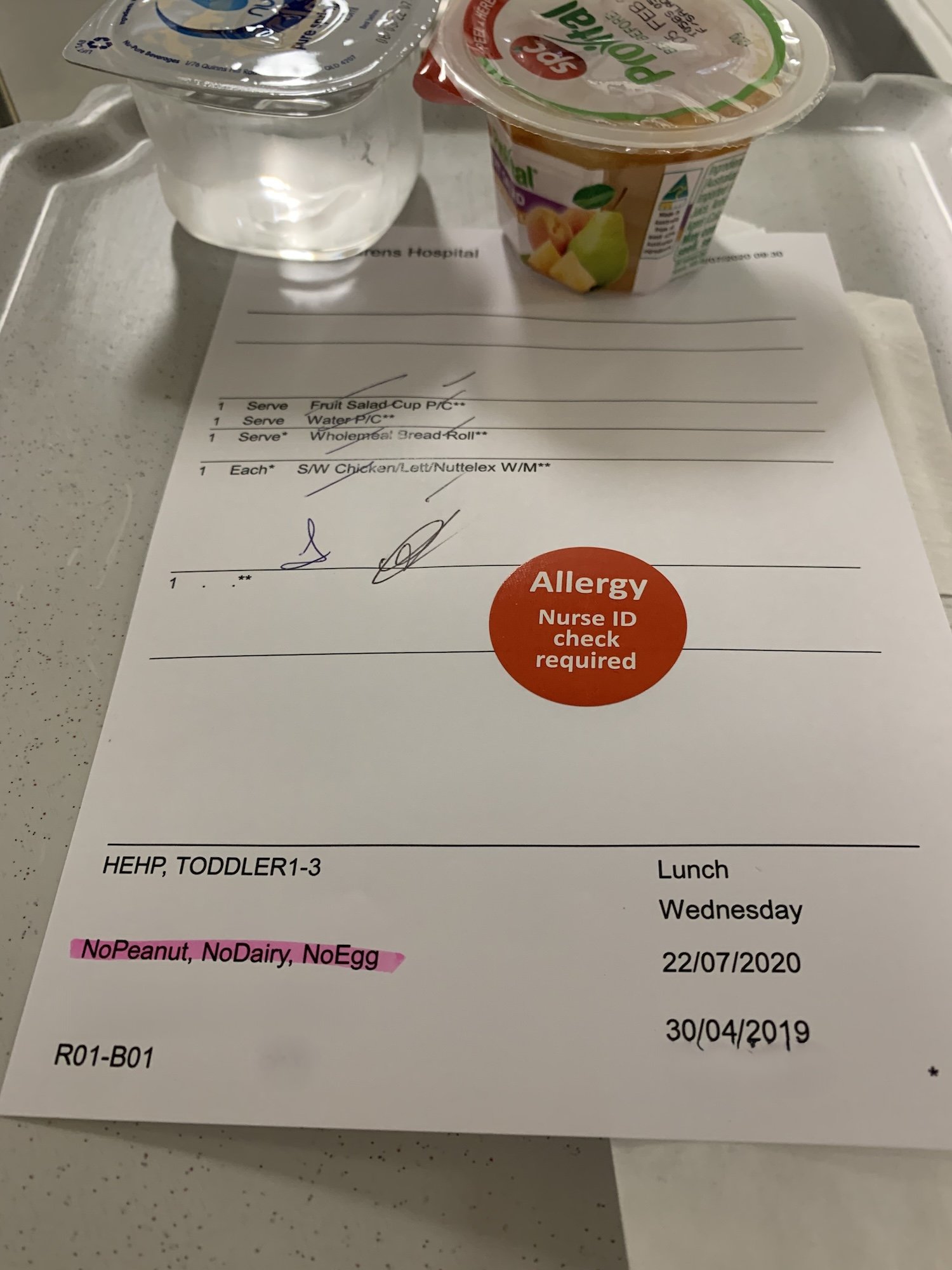
- Use a different coloured tray for food allergy meals and highlight food allergies on meal slips.
- Use a different coloured plate for dining room style eating.
3. Serve food allergy meals first, before any other meals are given out. This applies to trolley style delivery or dining room service. Giving meals to patients and residents with food allergies first means they won’t be given a ‘standard’ meal in error.
4. Check that it is the right meal for that patient or resident. Just like medications, giving the wrong meal or menu items to someone with food allergy can be dangerous. Best practice is to do a 3-point identification check and have another staff member check the meal is being given to the right patient or resident.
- Check that the patient’s or resident’s name, date of birth and MRN matches what is on the meal ticket.
- Check with the patient or resident or their caregiver that the food allergy recorded on the meal ticket is correct. If they say they have a different allergy, do not give that meal to the patient or resident. The allergy record should be updated straight away and a new meal prepared from the kitchen.
How does this work for aged care and residential care settings where there is no meal ticket or ID band? Only staff who know the resident with food allergy should give the resident their meal. Whoever is giving the meal to the resident should check with the foodservice staff (including the chef) that the meal has been made for the resident’s allergy.
5. Check that the items on the tray are correct. When meals are given to patients or residents with meal tickets or meal slips, staff should check that the items on the tray or plate match the items on the meal slip. The ingredient checks should have already been done in the kitchen so this staff member does not need to know all the ingredients. They just need to make sure that there is nothing extra on the tray that should not be there. For example, if the meal ticket says ‘spaghetti bolognaise, garden salad, fruit salad’ , check that only those items are on the tray.
If there is anything extra on the tray, especially if there is an item that obviously contains the person’s allergen, take it away and check with the kitchen that everything else on the tray is correct before giving the meal to the patient or resident.
If staff are not sure of the safety of the meal, they should speak to the foodservice staff.
6. Do not leave meals at the patient’s or resident’s bedside or at the table if they are not there. This goes for all patients or residents. Leaving meals at patients’ or residents’
bedsides or at their place in the dining room when they are not there increases the risk of wandering patients or residents eating meals that are not made specifically for them.
7. Supervise bulk meal deliveries, buffets and self serve. It is best practice to make an individual meal for patients or residents with food allergies. If your facility does serve meals for patients or residents with food allergy from bulk containers or a buffet, they should be served first, before anyone else. Staff must know which items in the bulk delivery or buffet are safe for those patients or residents, so they need to be able to read the ingredient and allergen content of each item at that mealtime. Meals must be dished up using different utensils for each item. When serving, prevent food from one bulk container dropping into another food.
8. Create a food allergen menu matrix for food and drinks kept outside the main kitchen. Patients and residents often need food and drinks from the pantry or from food and drink bays between meals and after hours. An up to date food allergen menu matrix lists the allergen content and ingredients of all foods and drinks kept in pantries so staff can check which items are safe for patients or residents with food allergies. If they can, staff should get a second staff member to check that the food is safe for the patient or resident with a food allergy.
These procedures will be slightly different for each hospital and aged care facility, but by following this list we can help keep patients with food allergies safe.
And just a side note – these strategies can be used for other high risk special diets! High risk special diets are for patients and residents who can have adverse events if they are given the wrong meal. Examples include patients on ‘metabolic’ diets for inborn errors of metabolism, ketogenic diets for epilepsy, or highly restrictive renal diets.
Make food allergen management training part of your staff training program. We have free All about Allergens online training courses for hospital and residential care staff that can be completed by foodservice, nursing, care and dietetic staff.
Got questions or comments on our article, or want to tell us how you manage food allergies in your facility to add to our best practice guidance? Contact us at info@nationalallergycouncil.org.au
Subscribe to the National Allergy Council newsletter for all the latest project updates: https://nationalallergycouncil.org.au/news#sub
Ingrid Roche is a National Allergy Council Senior Project Officer leading the National Allergy Council’s Foodservice Project and an Accrediting Practicing Dietitian specialising in food allergy and foodservice.